All Product
Product
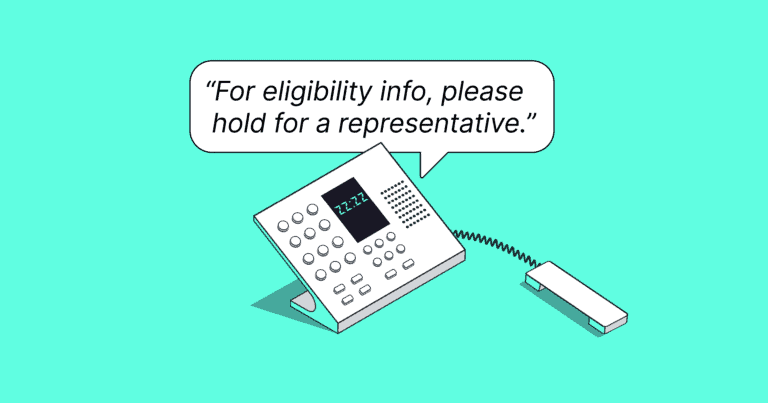
In September, the Centers for Medicare and Medicaid Services (CMS) announced a change that many initially missed: Medicare Administrative Contractors (MACs) will remove beneficiary eligibility information from their interactive voice response (IVR) systems by March 31, 2025. Some have already begun to do so. With this change, CMS aims to improve security, reduce fraud, and...

For healthcare workers already plagued by the burden of administrative overwhelm, repeatedly checking in on the status of a prior authorization adds to an already taxing clerical burden. And yet, it’s necessary – if these calls aren’t completed in a timely fashion, patients can face delays in treatment and providers risk losing revenue. That’s why...
Often, new solutions for call center staff claim that they’re powered by AI when in reality, they’re just hoping to capitalize on a buzzworthy phrase. At best, these tools may offer a simple wrapper around an existing GPT model and call it a day. This matters because GPT on its own cannot do what FastTrack™,...

We are excited to announce that FastTrack™, the first purpose-built AI copilot for healthcare, enters general availability today. FastTrack is an enterprise-ready AI copilot that enables healthcare staff, such as reimbursement specialists, to bypass tedious IVR systems and avoid hold times. This helps healthcare companies to save time so they can serve more patients. Whether...
Frequently, our customers have described the Infinitus AI agent as a super-productive member of their teams. And while we focus on creating products that augment busy healthcare workers – and don’t replace them – we understand why some think of our agent like a coworker. We’re officially in the era of “AI co-workers” after all. But...
AI agents are everywhere, with some news outlets proclaiming them to be the future of AI. We don’t disagree. At Infinitus, we talk a lot about our voice AI agents and fully digital AI agents, and the technology that powers them. Infinitus voice AI agents make phone calls to commercial and government payors on behalf...
Increasingly employer-sponsored plans are including copay accumulators, copay maximizers, or alternative funding sources as part of their plan design. In fact, estimates suggest about half of all lives covered by commercial insurance are enrolled in a plan that utilizes a copay accumulator and/or a maximizer. If your team is responsible for guiding individuals through coverage...

It’s just a phone call. What could be so complicated? At first consideration, conducting – and even automating – phone calls to major medical payors and pharmacy benefit managers (PBMs) to perform benefit verifications doesn’t seem as if it should be all that complex. After all, these calls are extremely common, extremely frequent, and entirely necessary....
While AI is dominating many conversations in healthcare, relatively few organizations in the space actually use generative AI tools, according to a recent survey. Among the primary reasons why are concerns about hallucinations, accuracy, and reliability. At Infinitus, we are committed to our mission of improving access, adherence, and affordability in healthcare – but along...
Picture today’s tech landscape as a pendulum in motion, swinging between two distinct poles. At one extreme, there’s a somewhat prevalent notion where AI not only equals, but eventually outshines human intelligence. On the other side, there’s a lingering concern that AI could displace human roles, rendering us obsolete. This narrative overlooks the fertile middle...
When it comes to prior authorizations (PAs), ePA or 278 solutions aren’t enough. It’s often challenging to resolve complex or time-sensitive prior authorizations electronically. Details such as PA status, denial reasons, and appeal options either aren’t readily available or the turnaround time is too long. In these cases, healthcare providers’ staff often manually call a...
When it comes to benefit verifications, ambulatory surgery centers are under intense pressure to turn around authorizations quickly. However, it’s not uncommon for this crucial task to take longer than expected. Coverage information online is often incomplete, and staff must make multiple calls to payors to close out inquiries and ensure procedural dates are met....

Healthcare executives in Pharmaceutical and Specialty Pharmacy industries are stuck between a rock and a hard place. Their staff is overwhelmed with a backlog of tasks, including calls to payors and PBMs to verify patient benefit information. While the status quo has been to hire more people, candidates are nowhere to be found and this...
San Francisco — May 16, 2023 — Infinitus Systems, Inc., the Conversational AI Platform for Healthcare, today announced that Gramercy Surgery Center, the #1 Ambulatory Surgery Center (ASC) in New York, has chosen Infinitus to automate tedious and time consuming tasks of insurance verification and prior authorization across its care sites. With Infinitus, Gramercy aims...

Today, my co-founder Shyam Rajagopalan and I are introducing the world to Infinitus, a voice robotic process automation (Voice RPA) company targeted to reduce the complexity and cost of healthcare in the United States. We have been working on this project since February 2019 and are excited to share our progress on it on this blog over the coming years.